445 out of every 100,000 tested immigrants come up positive for syphilis. Meanwhile, the FDA is now allowing the import of drugs for syphilis treatment…because American supplies are running low.
Last summer, doctors in Texas expressed concern that the illegal immigrants entering the nation as a result of Biden’s lax border control policies were not being tested for readily transmittable infectious diseases…like syphilis.
“CDC has comprehensive surveillance systems to track communicable diseases (diseases that can be transmitted to others) for people in the U.S.,” Bligh said. “However, CDC does not track diseases by immigration status.”
Between 2014 and 2019, approximately 445 out of every 100,000 tested immigrants and refugees were positive for some form of syphilis, per the CDC
The CDC website states that “syphilis tests must be performed at the time of the immigration medical examination and at the laboratory, as stated in the panel physician agreement,” — but some doctors are skeptical.
“They are not being tested for COVID as they come across [the border], much less for syphilis,” [James Hodges, M.D., an internist in Waco, Texas], told [Fox News contributor Dr. Marc Siegel].
…A spokesperson for the Texas Department of State Health Services told Fox News Digital on Thursday that they are unable to quantify the impact of immigration on reported syphilis cases in Texas.
Now, the Centers for Disease Control and Prevention (CDC) reports that the number of syphilis cases has surged to the highest level in more than seven decades.
A staggering 207,000 syphilis cases were reported in the US in 2022 — an 80% increase since 2018.
“The syphilis crisis in our country is unacceptable,” Health and Human Services Secretary Xavier Becerra declared in a press release on Tuesday, sounding the alarm over the “critical” public health crisis.
According to the CDC data, more than 170,000 syphilis cases were reported back in 1951. The number dropped dramatically after the widespread availability of antibiotics. By 1998, annual case numbers had dropped below 40,000 before creeping up again over the past two decades.
“In the United States, syphilis was close to elimination in the 1990s, so we know it’s possible to reverse this epidemic,” Dr. Jonathan Mermin, director of CDC’s National Center for HIV, Viral Hepatitis, STD, and TB Prevention, stated.
Public health officials assert it’s the lack of condom use and late screenings for syphilis that contribute to those numbers. And while that may be part of the problem, as the statistic cited above notes, 445 out of every 100,000 tested immigrants came up positive for syphilis.
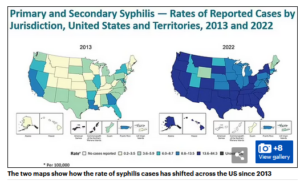
The Daily Mail maps out the issue in its article on this subject:
The untreated disease can lead to very serious health effects. The good news: Antibiotics are still an effective treatment.
Symptoms appear within three to four weeks of an infection and are often not noticed or dismissed as mild abrasions or heat rash.
The disease can then enter a second stage, where the sore disappears and is replaced with a rash that can last for weeks.
Without treatment, patients run the risk of the disease spreading to the brain and the spinal cord, which can cause complications including headaches, stroke, and meningitis — or inflammation of the brain’s protective linings.
There is particular concern over the disease in pregnant women because the bacteria can infect the placenta and developing infant — causing complications including vision and hearing loss and low birth weight.
Treatment for the disease involves administering antibiotic injections to patients.
The bad news is that the supply of treatment for syphilis is so low now that we must import the drugs from other countries.
The U.S. Food and Drug Administration will temporarily allow the import of a syphilis drug made by France’s Laboratoires Delbert, the company said on Wednesday.
Laboratoires Delbert said it was coordinating with the health regulator to bring stenciling into the United States to address syphilis drug shortages, according to the letter on the FDA’s website.
Syphilis has long been the scourge of humans. New research shows that mankind has been forced to contend with syphilis-like diseases for the past 14,000 years.
To better understand the history of treponemal disease in the Americas, Verena Schuenemann and Kerttu Majander, archaeogeneticists at the University of Zurich in Switzerland who led the 2020 study, and their colleagues looked for signs of treponemal bacteria in bone specimens of human remains buried some 2,000 years ago on Brazil’s southern coast.
The researchers found that the T. pallidum genomes recovered from the bones were most similar to those of the modern subspecies that usually cause bejel. This disease is not typically found in the Americas today. The ancient genomes were less similar to those of the strains usually associated with yaws or syphilis, which are both found in South America. This implies that the current distribution of T. pallidum subspecies differs from that of the past.
Further analysis of the genomes suggested that known T. pallidum lineages probably began to diversify as long as 14,000 years ago — 10,000 years earlier than previously suggested — and that modern strains evolved in the past 3,000. “It seems they have been accompanying us for a long time, which wasn’t expected,” says Schuenemann.
Living in the golden age of great medicine, with readily available drugs and containment of infectious diseases, was nice. Biden’s border crisis has brought this era to an end.
The untreated disease can lead to very serious health effects. The good news is that antibiotics are still an effective treatment.
Symptoms appear within three to four weeks of an infection and are often not noticed or dismissed as mild abrasions or heat rash.
The disease can then enter a second stage, where the sore disappears and is replaced with a rash that can last for weeks.
Without treatment, patients run the risk of the disease spreading to the brain and the spinal cord which can cause complications including headaches, stroke and meningitis — or inflammation of the brain’s protective linings.
There is particular concern over the disease in pregnant women because the bacteria can infect the placenta and developing infant — causing complications including vision and hearing loss and low birthweight.
Treatment for the disease involves administering antibiotic injections to patients.
The bad news is that the supply of treatment for syphilis is so low now that we must import the drugs from other countries.
The U.S. Food and Drug Administration will temporarily allow the import of a syphilis drug made by France’s Laboratoires Delbert, the company said on Wednesday.
Laboratoires Delbert said it was coordinating with the health regulator to bring extencilline into the United States to address syphilis drug shortages, according to a letter on the FDA’s website.
Syphilis has long been the scourge of humans. New research shows that mankind has been forced to contend with syphilis-like diseases for the past 14,000 years.
To better understand the history of treponemal disease in the Americas, Verena Schuenemann and Kerttu Majander, archaeogeneticists at the University of Zurich in Switzerland who led the 2020 study, and their colleagues looked for signs of treponemal bacteria in bone specimens of human remains buried some 2,000 years ago on Brazil’s southern coast.
The researchers found that the T. pallidum genomes recovered from the bones were most similar to those of the modern subspecies that usually causes bejel — a disease that is not typically found in the Americas today. The ancient genomes were less similar to those of the strains usually associated with yaws or syphilis, which are both found in South America. This implies that the current distribution of T. pallidum subspecies differs from that of the past.
Further analysis of the genomes suggested that known T. pallidum lineages probably began to diversify as long as 14,000 years ago — 10,000 years earlier than previously suggested — and that modern strains evolved in the past 3,000. “It seems they have been accompanying us for a long time, which wasn’t expected,” says Schuenemann.
Living in the golden age of great medicine, with readily available drugs and containment of infectious diseases, was nice. Biden’s border crisis has brought this era to an end.